Icebergs, navigation and sea level
In the old days, icebergs in the Antarctic could completely disrupt shipping routes. Today, the number of icebergs is directly linked to changes in sea levels.

How do skippers deal with the notion of time on a round the world race?
As we prepare to change time and move to summer time, we take a look at the perception of time, time differences and the relationship with the clock when you're so far offshore. Romain Attanasio (Fortinet-Best Western) and Éric Bellion (Stand as One) analyse this essential aspect of life on board.


How does the weather forecast work?
Weather is more than just an everyday conversation. It is based on sophisticated models and considerable technological advances. On this World Weather Day, let's take a look at the basics, which will help us to understand what skippers are experiencing around the world this winter.

Official supplier, Cougnaud builds over 5,000 m2 of temporary spaces
Cougnaud, builder of living and working spaces, continues to go beyond old conventions by rethinking the way we build. Fast, agile, responsible, limiting or neutralising the carbon impact of construction, Cougnaud is working to change the sector through off-site construction.

At the heart of winter refit: where do we stand with the job list?
For the IMOCA teams, winter means work in the yard. While the skippers are taking this much-needed time to rest, the technical teams are busy at work! The expression "job list" is on everyone's lips. With the Vendée Globe and two solo transatlantic races underway, there's no time to lose. But what…

UNESCO and the Vendée Globe: together for a better understanding of the ocean
As part of the United Nations Decade of Ocean Science for Sustainable Development (2021-2030), the Vendée Globe and UNESCO are joining forces to mark a new milestone after ten years of joint efforts between UNESCO and the IMOCA Class.

Discover the Antarctic with Polar Journal
From the Cape of Good Hope onwards, the Vendée Globe skippers will gradually come across the Southern Ocean, with its bodies of water circling Antarctica. To mark the occasion, the Vendée Globe and PolarJournal, a specialist news outlet on the polar regions, are bringing you on board to discover…
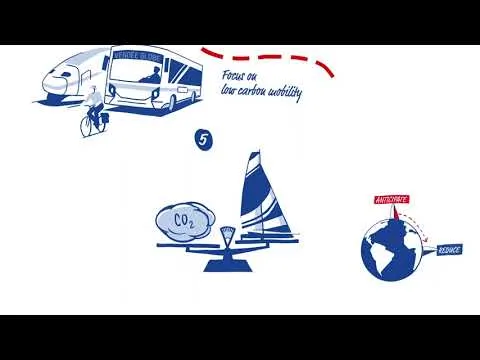

10 environmental commitments for 10th edition of the Vendée Globe
In the run-up to the 10th edition of the solo, non-stop, non-assisted round the world race, the Vendée Globe is affirming its environmental commitments. In addition to the causes supported by the skippers, the organization is also committed. The approach is part of a long-term perspective and is…

With Ifremer, scientists get into the race!
Scientists and sailors are keen to learn more about and preserve the ocean, which is under threat from climate change and plastic pollution. This commitment is underlined this year by the partnership between Ifremer and the Vendée Globe, aimed at raising awareness of the major challenges facing…

The TAAF Austral Islands: the Vendée Globe's ice gate
More than 250 years after the discovery of the Crozet and Kerguelen archipelagos by sailors Marc-Joseph Marion du Fresne and Yves-Joseph Kerguelen de Trémarec, the southern seas, situated between the roaring forties and the howling fifties, remain an exceptional and demanding area for exploration…

When the ocean connects to offshore racing
Created in 2021 on the initiative of Carole Saout-Grit, a physical oceanographer, Océans Connectés is an independent digital media entirely dedicated to marine sciences.

EMYN, a key player in the Vendée region, renews its partnership with the race
EMYN, the second offshore wind farm on the Atlantic coast and a key project for the French industry, due to come on stream in 2025, is renewing its partnership with the Vendée Globe. This collaboration symbolises a shared commitment to innovation, the environment, sustainability and the promotion…

New York Vendée - Les Sables d'Olonne: an international fleet at the start!
While the IMOCA are in winter refit, the organisers of the Vendée Globe are unveiling the details and line-up of their transatlantic race, the New York Vendée - Les Sables d'Olonne, which will start off the coast of the United States on 29 May 2024 at 2pm local time.